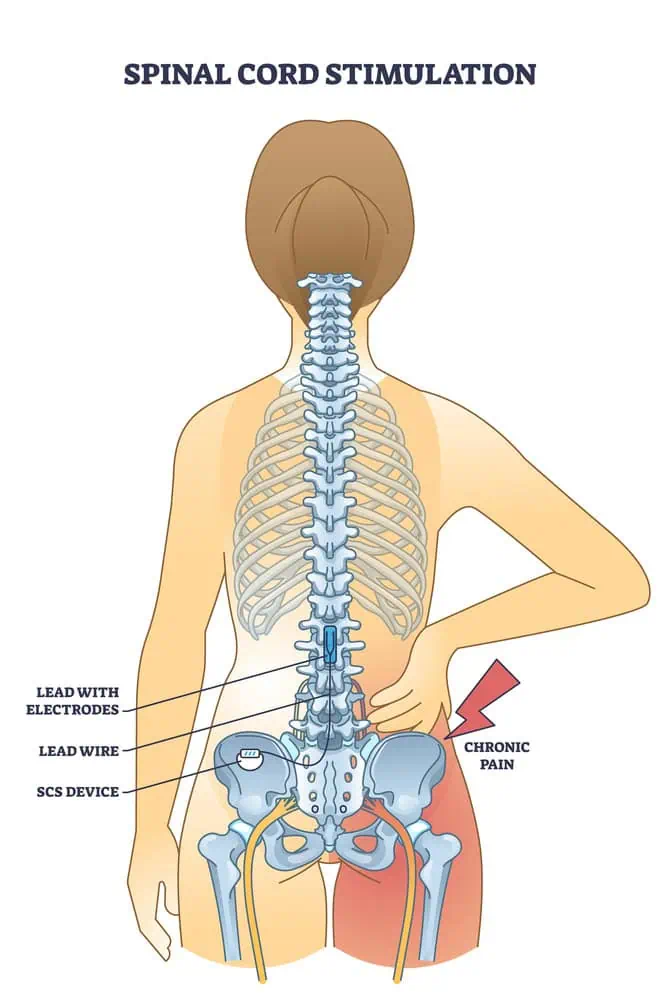
Spinal Cord Stimulation (SCS) is a therapeutic technique used to alleviate chronic pain by targeting nerve signals in the spinal cord. When medications or other treatments fail to provide relief, SCS offers a viable alternative for patients struggling with persistent pain, particularly in the lower back and limbs. This method involves the delivery of low-voltage electrical currents to interrupt pain signals on their way to the brain, potentially leading to a significant reduction in pain perception.

The technology behind spinal cord stimulation has evolved over the years, allowing for more sophisticated devices and improved patient outcomes. Candidates for SCS usually undergo a trial period to gauge the effectiveness of the therapy on their specific conditions. If successful, a permanent device is implanted through a surgical procedure. The implantable device, composed of a small generator and leads placed near the spinal cord, is adjustable to cater to the individual needs of each patient. It is a reversible treatment that can adapt to changes in pain or advancements in technology over time.
Key Takeaways
- SCS is used to manage chronic pain by modifying nerve signals in the spinal cord.
- A trial period precedes permanent device implantation to ensure effectiveness.
- The SCS system is customizable and updatable, with therapy reversible if necessary.
Fundamentals of Spinal Cord Stimulation
Spinal Cord Stimulation (SCS) is a sophisticated therapy that we administer to alleviate intractable pain by interrupting pain signals on their route to the brain. We use SCS after other non-surgical treatments have not provided the needed pain relief.
Mechanism of Action
Our approach with SCS involves sending electrical signals directly to the spinal cord via a small device that we implant near the spine. Precision is key; thus, we position electrodes meticulously along the dorsal column. These electrodes emit low-voltage electrical currents to modulate the pain signals before they reach the brain. The modulation provides a form of pain relief that is felt as a gentle tingling sensation, replacing the typical pain experience of patients.
Historical Perspective
The inception of SCS dates back to the 1960s, and since then, we’ve seen significant advancements in the technology. Initially, the application of SCS was limited and the understanding of its benefits rudimentary at best. Over time, we’ve refined both the hardware and our techniques to ensure more precise and effective outcomes. Our experience now allows for a tailored SCS therapy, where we customize electrical signals in terms of frequency and amplitude to suit individual patient needs — enhancing their quality of life and reducing dependency on pain medications.
Preparation for Spinal Cord Stimulation
When considering spinal cord stimulation (SCS) as a treatment option, careful preparation is crucial in ensuring the best outcomes. We focus on selecting the right patient and conducting thorough evaluations and imaging studies before proceeding with the procedure.
Patient Selection and Psychological Evaluation
It is imperative that we identify the right candidates for SCS therapy. Our pain specialists and doctors work together to evaluate patients in terms of their medical history, pain characteristics, and treatment response. A psychological evaluation is a vital component of this process, providing essential insight into the patient’s coping mechanisms, mental health status, and expectations regarding pain management. This assessment helps us ensure that candidates are mentally and emotionally equipped to undergo SCS treatment and manage their expectations.
Imaging and Diagnostic Studies
Before SCS device implantation, comprehensive imaging and diagnostic studies are necessary. We utilize MRI, X-rays, and CT scans to gain precise anatomical insights. These imaging studies allow us to assess the health of the spinal cord and surrounding areas, help rule out contraindications for SCS, and plan the procedure. Ensuring that the neurosurgery team has access to this accurate and up-to-date information is essential in planning the intervention path and determining the optimal placement of the stimulator leads.
The Spinal Cord Stimulator System
Spinal cord stimulators (SCS) are sophisticated devices implanted in the body to manage chronic pain by delivering low-level electrical pulses. These systems consist of multiple components that work together to modulate pain signals before they reach the brain.
Components of the System
The spinal cord stimulator system generally comprises three key components: the electrode leads, the pulse generator, and the remote control.
- Electrode Leads: Thin, insulated wires that end with electrodes. These are placed in the epidural space near the spinal cord to deliver electrical pulses.
- Pulse Generator: An implanted device, often referred to as the stimulator or battery, which generates the electrical pulses. It can be a conventional implantable pulse generator with a built-in battery, or a radiofrequency stimulator powered by an external source.
- Remote Control: Allows the user to turn the stimulator on and off, adjust the stimulation level, and sometimes program the generator to target specific pain areas.
Types of Spinal Cord Stimulators

There are various types of spinal cord stimulators tailored to different needs:
- Conventional Implantable Pulse Generators: These devices have a battery that usually needs to be surgically replaced every few years.
- Rechargeable Implantable Pulse Generators: Designed with rechargeable batteries that can last much longer than conventional batteries.
- Radiofrequency Stimulators: Typically used for more complex cases and do not require an implanted battery. They receive power from an external source.
- Dorsal Column Stimulators: Focus specifically on the dorsal regions of the spinal column to manage pain.
- Burst Stimulators: Among the newer devices, they deliver “burst” patterns of stimulation, believed to be more effective for certain patients.
Each device type offers unique features for pain management, and the choice depends on individual needs and the nature of their pain.
Clinical Applications
Spinal Cord Stimulation (SCS) is an advanced therapeutic method we resort to when addressing intractable chronic pain conditions. It offers significant hope to patients who have not found relief through conservative pain management techniques.
Indications for Use
We consider Spinal Cord Stimulation for patients who exhibit consistent and severe pain that has not responded to other treatments. These are typically individuals for whom invasive surgical options are deemed unpromising or too risky. The primary aim in using SCS is to alleviate persistent pain and improve the quality of life.
- Chronic Pain: When conservative therapies fail, SCS is a viable option for managing long-term pain.
- Complex Regional Pain Syndrome: We recommend SCS for mitigating the severe pain and discomfort associated with CRPS.
- Failed Back Surgery Syndrome (FBSS): For patients suffering from FBSS, SCS can provide a reduction in pain not achieved by previous surgical interventions.
- Back Pain: In cases of chronic back pain unalleviated by surgery or physical therapy, SCS may be beneficial.
Target Conditions
SCS targets specific conditions where neurostimulation has proven effective. We use SCS to modulate pain signals before they reach the brain, thereby reducing the perception of pain.
- Chronic Back Pain: SCS has shown effectiveness in reducing the intensity of chronic back pain in certain patients.
- Complex Regional Pain Syndrome (CRPS): SCS helps in managing the excruciating pain associated with CRPS, thereby improving limb function and quality of life.
- Failed Back Surgery Syndrome: For our patients with persistent pain after spine surgery, we find that SCS can significantly reduce their discomfort.
- Angina: We have observed that for refractory angina, SCS can be used to decrease the frequency and intensity of anginal attacks.
- Perineal Pain: We apply SCS therapy in managing perineal pain when other treatments fail to provide adequate relief.
By tailoring SCS therapy to individual needs, we strive to optimize pain relief and enhance patient functionality and well-being.
Surgical Procedure

In spinal cord stimulation (SCS), the surgical procedure is a critical component that comprises two main phases: an initial trial period to evaluate effectiveness, followed by the implantation technique for a permanent device if the trial is successful. Now, let’s discuss each phase in detail.
Trial Period
During the trial period, we temporarily insert a lead into the epidural space near the spine. This is typically done under local anesthesia, and sedation may be administered to ensure comfort. We use fluoroscopy, a type of real-time x-ray, to guide the placement of the temporary lead accurately.
Insertion of Lead:
- An incision is made near the middle of the back.
- The temporary lead is inserted into the epidural space above the dura mater.
Testing Effectiveness:
- After the lead placement, we connect it to an external trial stimulator.
- The patient is then asked to provide feedback on the level of pain relief during the trial period.
If the trial is successful, indicating significant pain relief, we plan for a permanent implant.
Implantation Technique
The implantation of a permanent device occurs only after a successful trial. This procedure is slightly more complex and involves placing a permanent lead and the stimulator device beneath the skin.
Preparation:
- Conducted under local anesthesia and sedation.
- A new incision is made, and a pocket is created to house the stimulator, typically in the buttock or abdomen.
Placement:
- The permanent leads are inserted into the epidural space using fluoroscopy.
- The leads are then anchored, and the device is connected.
Closure:
- We close the incisions with sutures.
- Care is taken to ensure everything is secure and placed properly to minimize movement and discomfort.
Post-implantation, the device settings are adjusted to optimize pain relief for the individual patient, and comprehensive care instructions are provided to ensure proper healing and function.
Postoperative Care and Recovery

Following spinal cord stimulator implant surgery, we emphasize two critical phases: managing the immediate postoperative period effectively and ensuring long-term management for optimal patient outcomes. Our approach targets not only the minimization of pain but also the enhancement of the overall quality of life.
Immediate Postoperative Period
In the hours following the surgery, we closely monitor our patients to manage pain and watch for any complications. It’s usual to feel some discomfort, and we typically prescribe medications to alleviate this. We instruct our patients to limit physical activity and ensure they understand the importance of sleep in their recovery. To support the healing process, we may cover the surgery site with a dressing or bandage, and advise patients on how to care for their incision.
- Pain Management: Administer prescribed pain medications as directed.
- Incision Care: Keep the surgical site clean and dry.
- Activity Limitations: Avoid heavy lifting and strenuous activity as advised.
Long-term Management
Long-term recovery involves a comprehensive plan that includes physical therapy, gradual engagement in physical activities, and ongoing pain management strategies. Our goal is to help our patients return to a fulfilling quality of life with appropriate adaptations.
- Physical Therapy: Begins with gentle exercises and progresses as per patient tolerance.
- Activity Resumption: Gradual increase in daily activities, with guidance on safe movements.
- Pain Management Adjustments: Regular assessments to fine-tune stimulation settings and medication doses.
We remind our patients that full benefit from the stimulator may take time but persisting with these guidelines typically leads to a significant improvement in daily functioning and comfort.
Complications and Troubleshooting
In spinal cord stimulation (SCS) therapy, complications can arise, but with careful management, many issues can be mitigated. Below, we explore common complications that might occur and delve into some of the device-related issues, providing insights on troubleshooting these problems.
Common Complications
Complications with SCS are varied, ranging from minor to severe. Infections can occur at the incision site or within deeper tissues and may require antibiotics or, in some cases, surgical intervention. Another risk is the development of hematomas or seromas, which are collections of blood or fluid, respectively. These conditions might lead to inflammation and additional complications if not addressed promptly.
Nerve injuries can happen during the implantation of the leads, potentially leading to pain or paralysis. Fortunately, such instances are rare. Occasionally, the electrodes shift from their original location, a complication known as migration, which can result in a loss of pain control or the sensation of jolting or shock.
Device-Related Issues
SCS devices, while sophisticated, are not immune to malfunctions. A malfunction may present as a sudden change in stimulation, loss of pain relief, or unusual sensations. It’s essential to assess and troubleshoot any device malfunction promptly.
Programming issues are the most frequent problems, usually resolvable through adjustments by a clinician. Battery failure or damage to the leads or the device itself can also contribute to inadequate pain control. In these cases, a replacement or repair of the component may be necessary.
In managing these events, we aim to ensure patient safety and maintain the efficacy of the therapy, taking definitive action to correct any issues arising from the SCS system.
Impact on Patients’ Lives

Spinal Cord Stimulation (SCS) has been a transformative approach in managing chronic pain, significantly altering the course of patients’ lives. Our focus here is on the pivotal changes it brings about in both physical discomfort and mental well-being.
Pain Management and Quality of Life
Through SCS, patients often experience a marked reduction in pain, which in turn dramatically enhances their quality of life. According to a Cleveland Clinic resource, this therapy primarily benefits those suffering from nerve pain, spine, or back pain. It is not unusual for individuals to report a decrease in their reliance on strong opioid-based painkillers, which carry considerable side effects and dependency risks. Patients describe the sensation from the stimulator as a mild tingling, which is preferable over debilitating pain.
Mental Health Considerations
SCS can influence mental health beyond the realm of physical symptoms. Living with chronic pain, conditions such as depression and anxiety are not uncommon. However, improvements in sleep and a dulling of chronic pain symptoms have been associated with spinal cord stimulation, offering a respite from the mental health strain. Studies highlighted by ScienceDaily shed light on the intersection between chronic pain relief from SCS and amelioration in insomnia, a common issue that exacerbates mental health challenges. As sleep improves, so does the overall mental health framework, signaling a ripple effect initiated by effective pain control.
Advancements in Technology
Spinal Cord Stimulation (SCS) technology has undergone significant changes, with newer devices that offer remote control capabilities and advanced battery systems.
Emerging Innovations
We’ve observed substantial development in electrode design, which now allows for more precise targeting of nerve fibers, potentially increasing the efficacy of SCS systems. Our look at the latest SCS systems reveals enhanced remote controlling options, granting patients an unprecedented level of autonomy in managing their pain. These remote controls are intuitive, secure, and have paved the way for greater flexibility in how SCS therapy is delivered and adjusted. Furthermore, improvements in battery technology are notable, with a trend toward rechargeable systems that provide longer life and smaller, more patient-friendly implants.
Future Research Directions
As we move forward, our focus is on the sustainability of newer technologies. Future pathways include the exploration of battery-free devices, harnessing energy harvesting methods. We also anticipate further innovation in wireless technologies to improve the remote management of devices. Ultimately, our goal is to refine these technologies for more robust functionality and increased patient comfort.
Patient Education and Support
We recognize that living with chronic pain is challenging, and spinal cord stimulation (SCS) can be a valuable part of your pain management strategy. Our aim is to provide comprehensive information and strengthen support networks to enhance your understanding and ability to cope with the condition.
Information Resources
We offer a variety of information resources to aid in the education of patients considering or currently undergoing SCS therapy. Our goal is to ensure that you are well-informed about the procedure, its benefits, and the lifestyle adjustments it entails.
- Spinal Cord Stimulation Patient Education Booklet: This detailed guide provides intricate insights into how SCS functions, including the role of the implanted lead and electrical pulses.
- Hospital and Clinic Websites: Trusted medical institutions such as Johns Hopkins Medicine provide valuable information on the functionality and benefits of SCS.
- Direct Consultation with Pain Specialists: We encourage patient consultations with our pain management doctors to discuss the suitability and potential outcomes of the therapy for your specific situation.
Community Support and Rehabilitation
Building a network of community support is key to a successful rehabilitation process post-SCS implantation. Participation in pain management programs can further assist in improving your quality of life.
- Support Groups: Connect with others who have experienced similar pain issues and share strategies for coping with the changes SCS brings to your physical activity.
- Physical Rehabilitation Programs: Working closely with a physical therapist can help you adapt to the device and maintain or improve your physical activity levels in a safe manner.
- Remote Monitoring: Advancements in SCS technology include the option for remote monitoring by your doctor, helping to ensure the device is functioning optimally and adjustments are made as needed for pain management.
Frequently Asked Questions
In this section, we provide clear, accurate responses to common inquiries concerning spinal cord stimulator (SCS) devices. Our goal is to help clarify any confusion or concerns you might have about SCS therapy.
What restrictions will I face after getting a spinal cord stimulator implanted?
After the implantation of a spinal cord stimulator, we typically advise patients to avoid bending, twisting, lifting heavy objects, or engaging in strenuous activities for several weeks to prevent device displacement and to ensure proper healing.
Are there any known complications associated with spinal cord stimulators?
Spinal cord stimulators have been linked to certain complications such as infection, bleeding, lead migration, or technical issues with the device. However, our priority is to mitigate these risks through careful surgical procedure and post-operative care.
How much does a spinal cord stimulator implant typically cost?
The cost of a spinal cord stimulator implant can vary widely based on factors such as healthcare provider, geographic location, and insurance coverage. It is a significant financial consideration that requires discussions with your insurance company and healthcare provider.
What should I expect during the recovery period following spinal cord stimulator surgery?
During recovery, you may experience pain at the incision site, and we will manage your discomfort with appropriate medications. Monitoring for signs of infection and attending follow-up appointments is crucial in the weeks following the procedure.
How effective are spinal cord stimulators in managing chronic pain, according to user reviews?
User reviews often reflect positive outcomes, with many individuals reporting significant reductions in chronic pain. Nevertheless, results can vary, and expectations should be based on a comprehensive evaluation of your condition and consultation with a pain specialist.
What are the potential downsides to using a spinal cord stimulator for pain management?
Some potential downsides of using a spinal cord stimulator include the need for additional surgeries for maintenance or complications, the sensation of tingling or paresthesia from the device, and the possibility that the system may not provide the expected level of pain relief.